
Why You Wake Up at 3am Every Night in Perimenopause (and What to Do About It)
If you’ve found yourself waking up at 3am with your heart racing, your mind spinning, and absolutely no sign of sleep returning, welcome to one of the most common (and most frustrating) symptoms of perimenopause.
You’re not imagining things. And no, you’re not going crazy. For thousands of women in their 40s and 50s, disturbed sleep, especially in the early morning hours—is one of the earliest and most disruptive signs that hormones are shifting.
But what’s actually causing it? Why 3am? And more importantly, what can you do about it?
Let’s dive into the science behind perimenopausal sleep disruption and explore practical, research-backed strategies to help you sleep through the night again.
The 3am Wake-Up Call: What's Really Going On?
While occasional poor sleep is normal at any age, waking up at the same time every night, especially between 2am and 4am, is often hormonal. During perimenopause, your body's once-reliable rhythm starts to change, and the delicate balance between estrogen, progesterone, cortisol, melatonin, and insulin begins to wobble.
Estrogen and progesterone both support sleep. Estrogen helps regulate body temperature and serotonin production (your feel-good, calming neurotransmitter), while progesterone has natural sedative effects. When both start to decline, it affects your nervous system, your ability to regulate blood sugar, and your body’s ability to stay asleep.
Add in a sudden cortisol spike, the stress hormone that’s meant to wake you up in the morning, and you’ve got a recipe for the 3am wide-eyed stare at the ceiling.
Common Causes of 3am Waking in Perimenopause
1. Hormonal Fluctuations
Estrogen and progesterone fluctuate dramatically during perimenopause, and these changes affect every part of your sleep cycle. Estrogen helps regulate temperature and mood, while progesterone is calming and helps you stay asleep. When they drop suddenly (as they often do in early to mid-perimenopause), sleep becomes fragmented and unpredictable.
2. Cortisol Spikes
Cortisol, your stress hormone, should be low at night and gradually rise before morning. But in perimenopause, many women experience what’s called "early cortisol awakening response," where cortisol spikes too early, around 2am to 4am, causing you to wake up feeling alert, anxious, or wide awake for no reason.
3. Blood Sugar Drops
If you eat high-sugar or carb-heavy meals in the evening, or skip dinner altogether your blood sugar may dip too low overnight. This triggers adrenaline and cortisol release to raise your blood glucose, often waking you up in a panic.
4. Night Sweats or Hot Flushes
Estrogen helps regulate body temperature. When it declines, you’re more prone to overheating at night, which can trigger night sweats and wakefulness, particularly in the early morning hours when your body temperature is naturally starting to rise again.
5. Melatonin Disruption
Melatonin is your sleep hormone. It naturally declines with age, and is closely regulated by both estrogen and exposure to light. Without enough melatonin, falling asleep may not be the issue, but staying asleep becomes harder, especially in the second half of the night.
Why It’s Always Around 3am
Your sleep cycle is regulated by your circadian rhythm, which controls hormone production throughout the night. Cortisol levels are lowest between 10pm and 2am, then begin to rise toward morning. If cortisol rises too early, say, at 3am instead of 6am, it pulls you out of deep sleep and into wakefulness.
At the same time, blood sugar is naturally lower overnight. If you’re not eating in a way that supports stable blood sugar, or your liver isn’t functioning optimally, it may signal the brain to “wake up and fix it.”
Essentially, 3am is a perfect storm of hormonal shifts, stress chemistry, temperature sensitivity, and metabolic changes. That’s why so many women in perimenopause report waking up around the same time each night, unable to get back to sleep.
The Long-Term Impact of Sleep Disruption
Chronic sleep loss is more than just annoying; it affects everything from mood and memory to metabolism and immunity. It also makes other perimenopausal symptoms worse: weight gain, anxiety, hot flushes, and even inflammation.
Sleep loss in midlife is also linked to increased risk of insulin resistance, osteoporosis, cardiovascular disease, and cognitive decline. This isn’t about vanity or productivity, it’s about protecting your long-term health and quality of life.
What You Can Do About It: 9 Evidence-Based Solutions
The good news? You can absolutely improve your sleep with targeted, hormone-supportive strategies. Here’s what works best:
1. Balance Blood Sugar Before Bed
Include a protein-rich snack with a little healthy fat in the evening, like Greek yogurt with chia seeds, a boiled egg with avocado, or a collagen hot chocolate. Avoid sugary desserts or wine within 2–3 hours of bed, which can spike then crash blood sugar.
2. Try Magnesium Glycinate
Magnesium supports nervous system relaxation, balances blood sugar, and promotes deeper sleep. Magnesium glycinate (300–400mg at night) is best for calming the brain and muscles without causing loose stools.
3. Cool Your Room
Sleep experts agree: your bedroom should be around 16–18°C. Use lightweight bedding and moisture-wicking sleepwear. A cooling gel pillow or fan can help reduce night sweats and temperature spikes.
4. Support Your Adrenals with Adaptogens
If stress is contributing to your wakefulness, herbs like ashwagandha or rhodiola may help balance cortisol levels. These adaptogens support a more stable circadian rhythm and reduce that “wired but tired” feeling.
5. Use a Blue Light Filter After 7pm
Melatonin is extremely sensitive to light. Switch off bright overheads, avoid phone screens close to your face, or wear blue light–blocking glasses in the evening to support natural melatonin production.
6. Try a Collagen + Magnesium Bedtime Drink
Collagen provides glycine, an amino acid shown to improve sleep latency and nighttime recovery. Combined with magnesium and a pinch of sea salt, it makes an ideal hormone-friendly nighttime beverage.
7. Reduce Evening Stress
Give your body a “buffer zone” before sleep. Try stretching, journaling, breathwork, or a warm bath with Epsom salts. Avoid scrolling social media or responding to emails right before bed.
8. Consider Bioidentical HRT
If you’re struggling with persistent insomnia and other hormone symptoms, speak to your GP or integrative practitioner about hormone replacement therapy. Rebalancing estrogen and progesterone can significantly improve sleep, energy, and quality of life for many women.
9. Get Morning Sunlight
10–15 minutes of early morning sunlight helps anchor your circadian rhythm and tells your body when to release melatonin later that evening. Step outside with your tea or take a short walk, even if it's cloudy.
When to Seek Help
If you’ve tried everything and you’re still waking up regularly at 3am, it’s time to dig deeper. Consider checking:
-
Hormone levels (especially estrogen, progesterone, and cortisol)
-
Iron and B12 levels (especially if fatigue or anxiety are also present)
Sometimes underlying deficiencies or imbalances can mimic or worsen perimenopausal symptoms. A holistic practitioner can help identify the root cause and create a personalised support plan.
Final Thoughts: Sleep Isn’t a Luxury, It’s a Lifeline
Waking up at 3am every night doesn’t mean you’re broken, it means your body is asking for support. These disruptions are your hormones trying to rebalance themselves in a season of transition. The key is learning how to listen and respond with strategies that work with your biology, not against it.
You deserve to sleep deeply, wake up refreshed, and move through this midlife chapter with clarity, calm, and energy. And with the right tools, that’s absolutely possible.
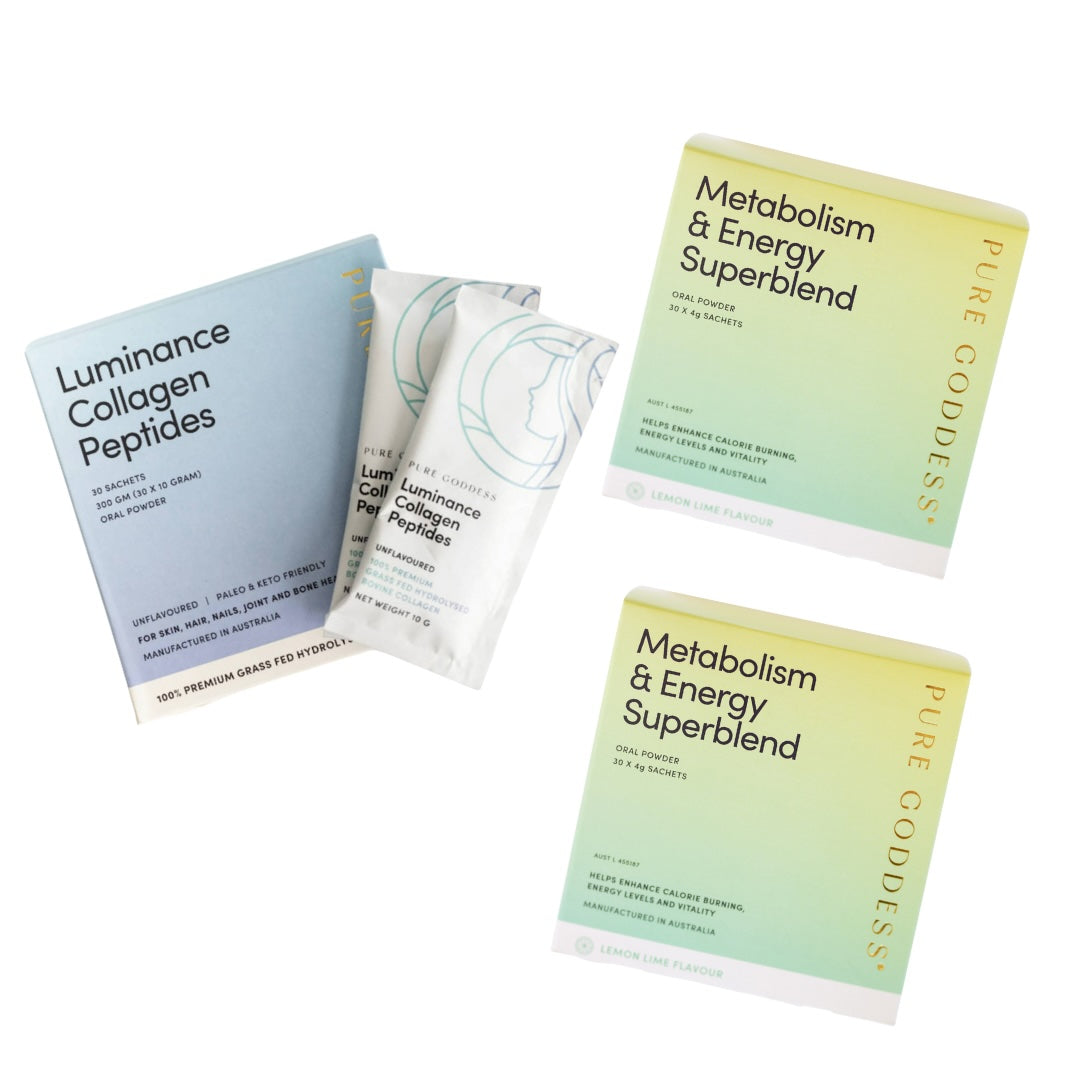
At Pure Goddess, we support women like you with science-backed supplements, hormone-friendly nutrition, and expert guidance to help you sleep better, feel better, and thrive in midlife, not just survive it.
Are you navigating the challenging and often confusing journey of perimenopause? Our eBook, Perimenopause Symptom Checker, is here to help. This comprehensive guide is designed to shed light on the symptoms that many women experience during perimenopause, offering clarity, practical advice, and support for every step of the way.






1 comment
My doctor said that as I am not having hot flushes my night waking is not related to perimenopause. Is this true?
Mel Magee
Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.