
Managing Insulin Resistance in Perimenopause: A Guide to Balancing Hormones and Supporting Health After 40
How to balance weight gain and hunger hormones after the age of 40.
Navigating the changes that come with perimenopause and menopause can be challenging. For many women over 40, these years introduce unique concerns such as weight gain, hormone imbalance, and a heightened risk of insulin resistance. This blog post is here to help you understand insulin resistance, its connection to perimenopause, and the actionable steps you can take to support your body.
Managing insulin resistance during perimenopause doesn’t have to feel overwhelming. With the right knowledge and tools, you can build habits that help you feel healthier, more balanced, and more in control.
What Is Insulin Resistance and Why It Matters in Perimenopause?
During perimenopause, the body undergoes hormonal shifts that affect nearly every system, including metabolism and blood sugar regulation. Insulin resistance occurs when your body’s cells stop responding effectively to insulin, a hormone responsible for managing blood glucose levels. When cells become less responsive, insulin builds up in the blood, leading to elevated glucose levels. Over time, this can lead to unwanted weight gain and increase your risk of developing type 2 diabetes.
In perimenopause, declining estrogen levels can contribute to insulin resistance, making it even more challenging to manage weight and maintain steady blood sugar levels. Addressing insulin resistance is crucial for overall health and can also improve energy levels, mood, and quality of life.
Recognising the Symptoms of Insulin Resistance in Perimenopause
Insulin resistance can present subtly, especially at the onset. Some common signs include:
- Increased abdominal fat or difficulty losing weight
- Persistent cravings, particularly for sweets or refined carbohydrates
- Feeling fatigued after meals
- Brain fog and difficulty concentrating
- High blood pressure and cholesterol levels
If you notice these symptoms, consider them as signals to start making adjustments to your lifestyle that can help improve insulin sensitivity. Here are some supportive, evidence-based lifestyle changes you can implement.
Lifestyle Adjustments to Manage Insulin Resistance After 40
1. Nourish with Balanced Nutrition for Steady Blood Sugar
Proper nutrition is one of the most effective ways to improve insulin sensitivity. Here’s how to structure your diet:
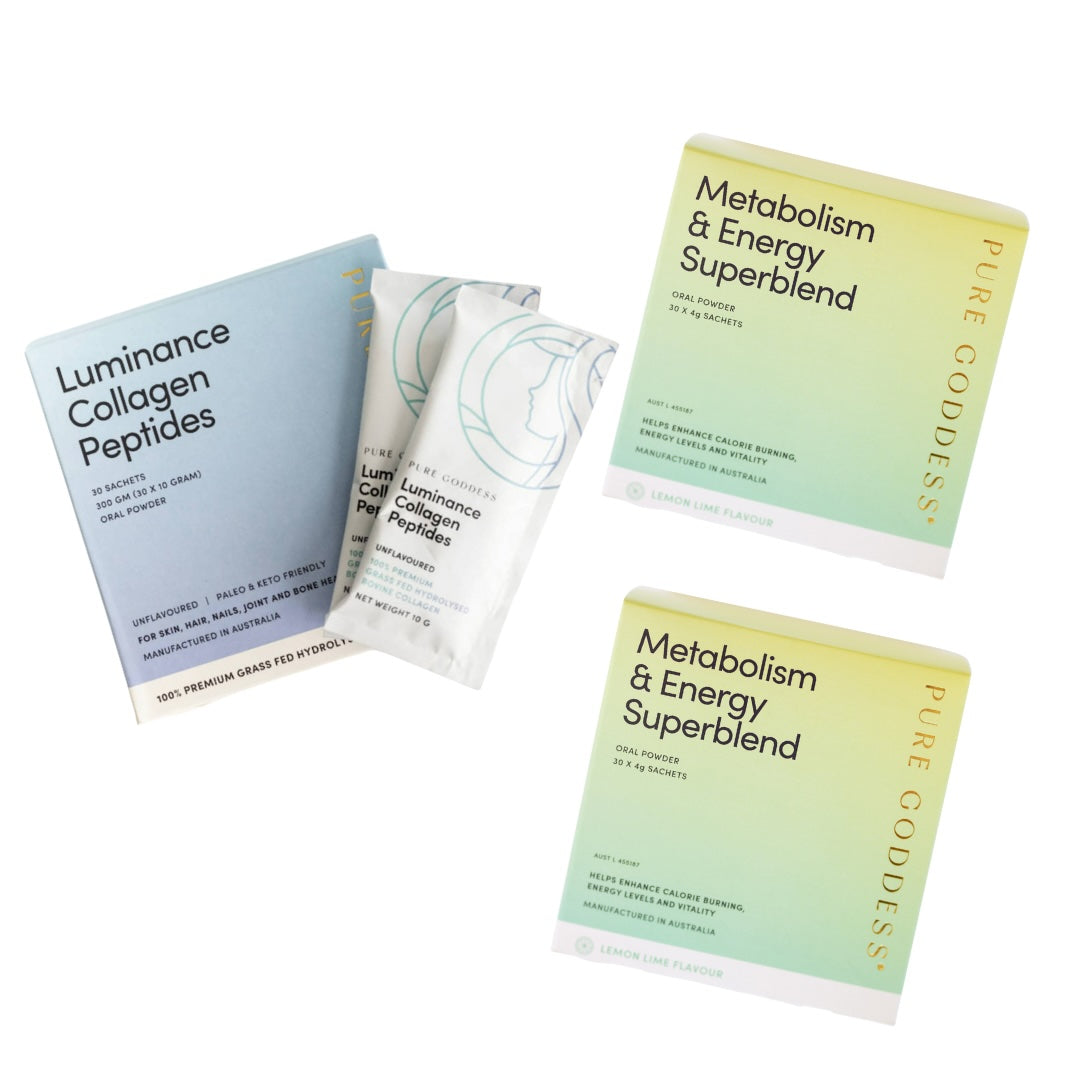
Fiber-Rich Foods: Fiber slows glucose absorption and helps maintain stable blood sugar levels. Incorporate fiber-rich foods like whole grains, legumes, and vegetables in every meal. Our best-selling Metabolism & Energy Superblend contains a highly soluble plant fiber and helps support healthy blood glucose levels - it is a great option if you are struggling to get enough fiber in your diet.
Lean Protein and Healthy Fats: Protein and healthy fats slow down digestion, reducing blood sugar spikes. Lean meats, fish, eggs, nuts, and seeds are great choices.
Low Glycemic Index (GI) Choices: Foods with a low glycemic index (like oats, lentils, and most vegetables) have a slower effect on blood sugar, making them ideal for keeping insulin levels in check.
Limit Processed Foods: Processed foods often contain added sugars and refined carbohydrates that can spike blood sugar and worsen insulin resistance. Instead, focus on whole, minimally processed foods that nourish and support balanced hormones.
Sample Meal Plan Example:
Consider a meal that includes baked salmon with quinoa and roasted vegetables, or a hearty salad with leafy greens, chickpeas, avocado, and a handful of nuts. Small adjustments like these can help you feel fuller for longer and maintain steadier blood sugar levels.
Take a look at our 28 Day Metabolic Reset Downloadable eBook - it is packed with low carb, insulin friendly recipes and advice.

2. Make Movement a Daily Habit
Regular physical activity is a proven method to improve insulin sensitivity. It doesn’t require intense workouts; consistent movement, even if gentle, can yield significant benefits.
Strength Training: Building muscle improves your body’s ability to use glucose, helping regulate insulin. Exercises like weightlifting, resistance bands, or body-weight exercises are beneficial.
Walking and Aerobic Activity: A brisk daily walk or light jogging, biking, or swimming helps reduce insulin resistance and promotes cardiovascular health, which is essential during perimenopause.
Mindful Movement: If traditional workouts aren’t appealing, activities like yoga, Pilates, or even dance can help maintain insulin sensitivity and are often gentler on joints, making them ideal for women over 40.
Start with manageable goals, such as walking for 15–20 minutes daily, and gradually increase as it feels comfortable. Consistency is key to reaping the long-term benefits.

3. Prioritize Restful Sleep for Hormone Balance
Quality sleep is essential for healthy insulin function and hormone balance. During perimenopause, fluctuating hormones can disrupt sleep, making this an area of focus for improving overall wellness.
Establish a Sleep Routine: Go to bed and wake up at the same time each day. A consistent sleep schedule helps regulate circadian rhythms, which positively influences insulin sensitivity.
Create a Relaxing Evening Ritual: Avoid stimulants like caffeine late in the day, and limit screen time at least an hour before bed. Try reading, gentle stretching, or deep breathing to wind down and prepare for restful sleep.
Manage Environmental Factors: Keep your bedroom dark, cool, and quiet. A comfortable environment promotes better quality sleep, which can make a significant difference in managing insulin resistance.
If you are struggling with getting to sleep or staying asleep which is incredibly common during perimenopause and menopause have a read of our blog post - 7 solutions for insomnia in perimenopause.

4. Use Stress Management Techniques to Lower Cortisol
Stress elevates cortisol levels, which can interfere with insulin regulation. Lowering stress can support hormone balance and reduce insulin resistance.
Mindfulness and Meditation: Short meditation sessions (even just 5–10 minutes) can effectively reduce stress. Guided meditation apps or deep breathing exercises can be helpful for beginners.
Journaling and Reflection: Writing down your thoughts can provide mental clarity and reduce stress. Setting aside a few minutes daily to journal can help you manage stress and emotions.
Engage in Enjoyable Activities: Carve out time for hobbies or activities that bring joy. Whether it’s gardening, painting, or cooking, doing what you love is a natural way to lower stress.

When to Seek Professional Support
Everyone’s journey through perimenopause is unique, and some may benefit from professional guidance. A registered dietitian or endocrinologist can help create a personalized approach to managing insulin resistance, considering factors like family history, lifestyle, and specific health goals. With individualized support, you can develop a comprehensive plan that addresses insulin resistance and promotes long-term health.
Perimenopause can bring new challenges, but it’s also an opportunity to reconnect with your body in a supportive way. By focusing on balanced nutrition, regular movement, quality sleep, and stress management, you can manage insulin resistance and maintain a healthy weight. With patience and self-compassion, these lifestyle adjustments will empower you to navigate this life stage with resilience and strength, building a foundation for lasting health and well-being beyond 40.



Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.