
The Truth About Fibroids
If you've ever heard the word "fibroids" and instantly felt your stomach drop a little, you're not alone. These common, non-cancerous growths often get talked about in hushed tones, like some mysterious menace lurking in the uterus, wreaking havoc on hormones, periods, and peace of mind.
But the truth is, fibroids are not some rare medical mystery. They affect up to 70% of women by the age of 50. And yet, many women don't fully understand what they are, why they happen, and what they can do about them.
So let’s break it down, science-backed, myth-busting, and compassionate. Because midlife is hard enough without vague health anxiety about something your doctor barely explains in a rushed 10-minute appointment.
What Are Fibroids?
Fibroids (also called leiomyomas or myomas) are non-cancerous growths made up of muscle and fibrous tissue that develop in or around the uterus. They can be as small as a seed or as large as a melon. Yes, really.
There are several types of fibroids, depending on where they grow:
-
Intramural fibroids grow within the muscular wall of the uterus.
-
Subserosal fibroids project to the outside of the uterus.
-
Submucosal fibroids grow into the inner cavity and are most likely to cause heavy bleeding.
-
Pedunculated fibroids are attached by a stalk to the uterine wall or surface.
While they are almost always benign, they can cause a wide range of symptoms, some subtle, some life-disrupting.
What Causes Fibroids?
This is where things get a bit complex. There isn’t one single cause, but rather a combination of factors:
1. Estrogen and Progesterone Levels
Fibroids are hormonally sensitive. They tend to grow during the reproductive years and often shrink after menopause. High estrogen (especially unopposed by progesterone) appears to play a key role in stimulating fibroid growth.
This is one reason why fibroids can flare up during perimenopause, when hormone levels fluctuate dramatically and estrogen dominance is common.
2. Genetics
Family history matters. If your mother or sister had fibroids, you’re more likely to develop them too. Some studies have identified specific genetic mutations in fibroid tissue, suggesting a strong hereditary component.
3. Race and Ethnicity
Women of colour are disproportionately affected, both in prevalence and severity. Research shows they are 2 to 3 times more likely to develop fibroids, and often experience symptoms earlier, with larger and more numerous growths.
4. Environmental and Lifestyle Factors
Endocrine-disrupting chemicals (like those found in plastics, pesticides, and non-stick cookware) may mimic estrogen and contribute to fibroid development. High stress, poor diet, and low levels of physical activity may also play a role.
When Do Women Get Fibroids?
Fibroids can technically develop at any age after puberty, but they are most commonly diagnosed between the ages of 30 and 50. Many women first discover them during perimenopause, when hormonal shifts start causing more obvious symptoms.
Interestingly, some women have fibroids for years without ever knowing it. They may only become apparent when a woman:
-
Experiences heavy or prolonged periods
-
Has difficulty conceiving
-
Feels pressure or bloating in the lower abdomen
-
Has a pelvic ultrasound for another reason
Common Symptoms of Fibroids
Not all fibroids cause symptoms. But when they do, it can seriously affect your quality of life. Here are the most common signs to watch for:
-
Heavy or prolonged menstrual bleeding
-
Pelvic pain or pressure
-
Frequent urination or difficulty emptying the bladder
-
Painful sex
-
Lower back pain
-
Constipation
-
Bloating or visible abdominal swelling
-
Fatigue or anaemia from chronic blood loss
One of the most distressing aspects for many women is the normalisation of these symptoms. Being told “you’re just getting older” or “it’s just part of being a woman” does not help. If your period is so heavy you're changing protection every hour, you deserve better answers, and better options.
Are Fibroids Dangerous?
This is the most common question, and the answer is mostly reassuring.
Fibroids are almost always non-cancerous, and very rarely (less than 1 in 1,000 cases) develop into a cancerous tumour called a leiomyosarcoma. There is no known way to predict which fibroids might become cancerous, though rapid growth, especially after menopause, should always be investigated.
However, just because fibroids aren’t usually dangerous doesn’t mean they’re harmless. Chronic bleeding can lead to iron deficiency anaemia. Large fibroids can distort the uterus, cause pain, pressure on organs, and in some cases interfere with fertility or pregnancy.
What Can You Do About Fibroids?
Luckily, we’re not powerless. There are a range of strategies, from dietary changes and supplements to medication and surgery. The best approach depends on your symptoms, your age, whether you're planning a pregnancy, and how close you are to menopause.
1. Watchful Waiting
If fibroids aren’t causing symptoms, many doctors recommend simply monitoring them. They often shrink after menopause when estrogen levels decline naturally.
However, even “silent” fibroids should be tracked with occasional imaging if they are large or growing.
2. Hormonal Treatments
If symptoms are moderate, hormonal therapies can help manage them:
-
Combined oral contraceptives: Regulate bleeding but don’t shrink fibroids.
-
Progestins (like the Mirena IUD): Reduce bleeding and may shrink fibroids slightly.
-
GnRH agonists: Induce temporary menopause and shrink fibroids, but are usually used short-term due to side effects like bone loss.
-
SPRMs (Selective Progesterone Receptor Modulators): Newer drugs that can shrink fibroids and control bleeding.
Each of these has pros and cons and should be discussed in detail with a specialist.
3. Non-Hormonal Medications
-
Tranexamic acid: Helps reduce menstrual bleeding.
-
NSAIDs: Manage pain and reduce inflammation but don’t affect the fibroids themselves.
4. Surgical Options
If fibroids are severely affecting your life, surgery may be necessary:
-
Myomectomy: Surgical removal of fibroids, preserving the uterus.
-
Hysterectomy: Complete removal of the uterus, which permanently eliminates fibroids.
-
Uterine Fibroid Embolisation (UFE): A minimally invasive procedure that blocks blood flow to the fibroids, causing them to shrink.
Newer techniques like radiofrequency ablation and focused ultrasound therapy are also being used with promising results, especially for women who want to avoid major surgery.
Can Natural Remedies and Lifestyle Changes Help?
Yes, especially if your symptoms are mild to moderate. While these won’t make fibroids disappear, they can slow growth, reduce inflammation, and help manage symptoms.
Diet
-
Anti-inflammatory foods: leafy greens, berries, nuts, oily fish. Take a look at our 7 Day Anti-Inflammatory Cleanse Ebook - This carefully curated 7-day plan is packed with anti-inflammatory foods that work together to soothe your system, restore balance, and support overall well-being.
-
Limit red meat and processed foods: These may raise estrogen and promote inflammation.
-
Increase cruciferous vegetables: broccoli, cauliflower, kale, all support estrogen detox.
Supplements
-
Vitamin D: Deficiency is linked with fibroid growth. A 2020 study showed that adequate vitamin D levels can inhibit fibroid cell proliferation. Read more about Vitamin D in our new blog: The Importance of Vitamin D for Australians: Sun Safety and Optimal Health
-
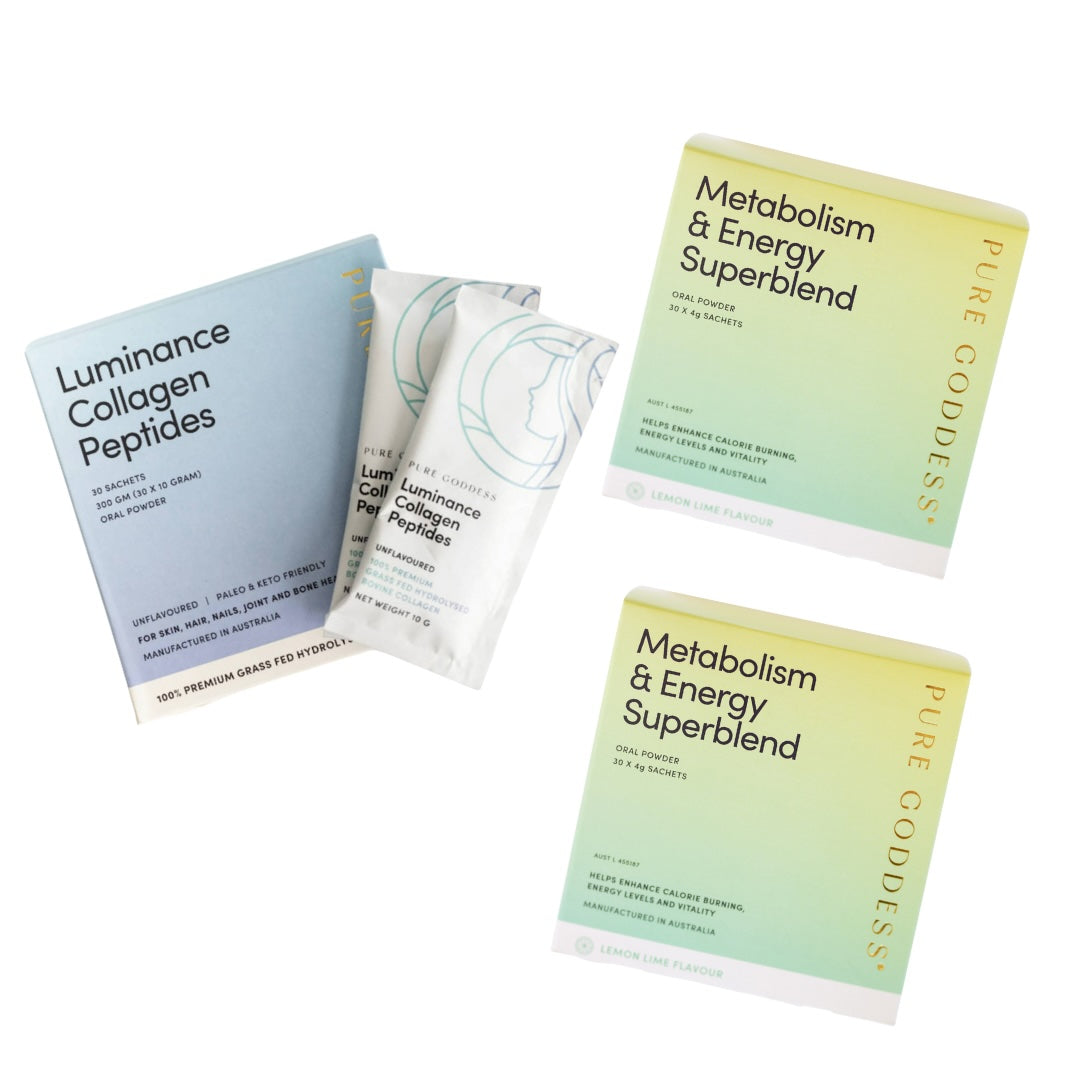
Green tea extract (EGCG): Shown in several studies to reduce fibroid size and improve symptoms over time. Metabolism & Energy Superblend
-
DIM (Diindolylmethane): Supports healthy estrogen metabolism.
-
Curcumin: The active compound in turmeric, with anti-inflammatory and anti-proliferative properties.
Always talk to your healthcare provider before starting supplements, especially if you’re on other medications.
Stress Reduction
Chronic stress can worsen hormone imbalance. Yoga, meditation, acupuncture, or simply regular downtime can help balance cortisol and support overall hormonal health.
What About Fibroids in Perimenopause?
This is where things get particularly tricky. During perimenopause, estrogen levels spike and dip unpredictably, making fibroids flare up for some women just before they were expecting relief.
It’s not unusual to experience the worst fibroid symptoms in your early 40s, only to see them resolve naturally once you reach full menopause. This is why many practitioners will suggest a conservative approach if menopause is within reach, unless symptoms are unbearable.
Final Thoughts:
Fibroids Are Common, But Not Something You Have To Just Live With
Fibroids are a part of life for many women, especially in midlife. But they’re also one of the most misunderstood, and under-discussed, health issues we face.
The good news? There are more options today than ever before. From natural supplements and lifestyle changes to surgical innovations and hormone therapy, there’s a path forward that doesn’t involve silent suffering or being told to “just wait it out.”
If you suspect fibroids are affecting your health, trust your instincts. Track your symptoms. Ask for a transvaginal ultrasound. Find a practitioner who takes your concerns seriously.
Your body is not broken; it’s giving you information. And with the right support, you can move through this phase with knowledge, confidence, and power.








Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.